
An autoclave serves as an essential sterilization device in healthcare settings while correct usage maintains high medical standards.
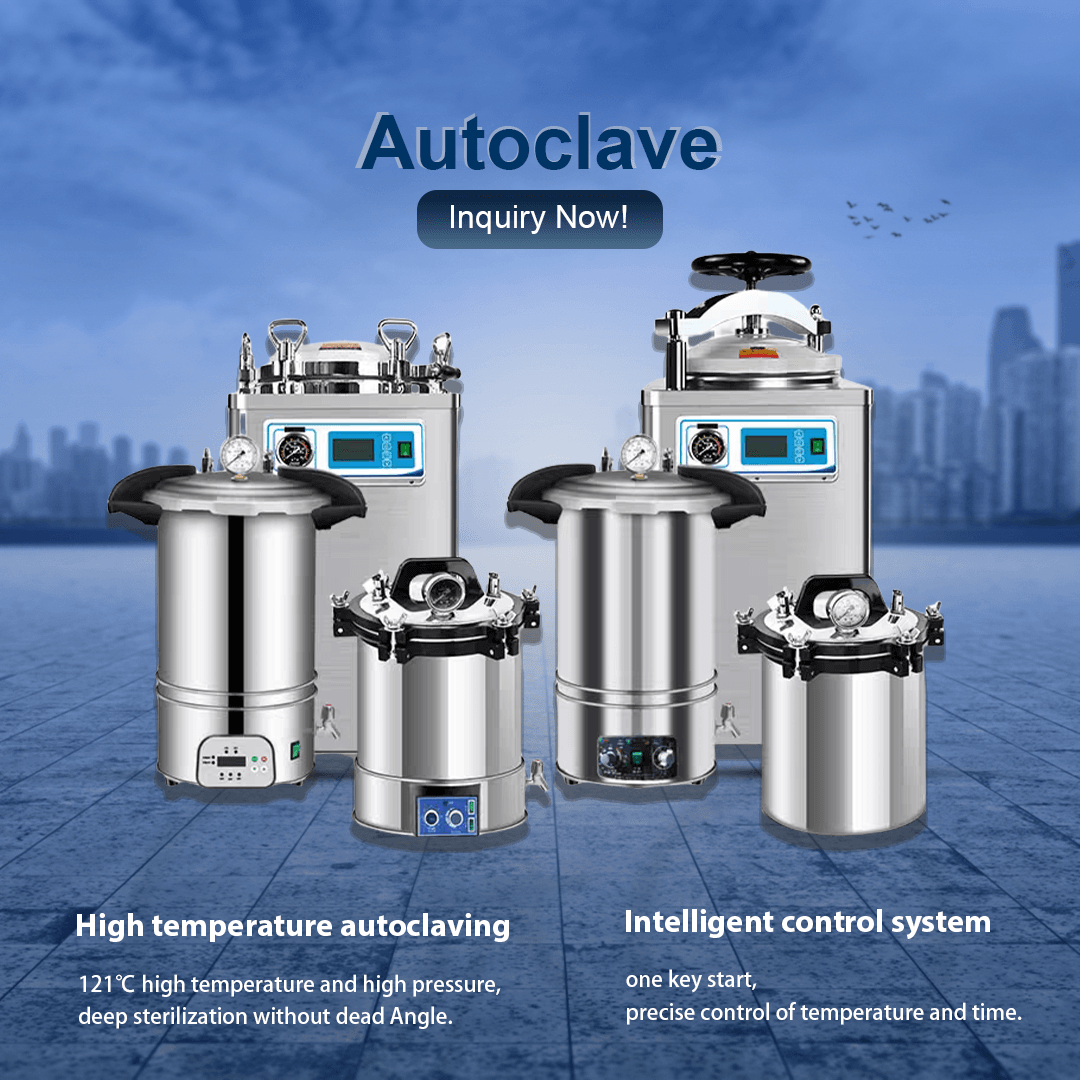
Healthcare environments use autoclaves to sterilize medical instruments and materials by killing all microbial life forms such as bacteria, viruses, fungi, and resistant spores with high-pressure steam. This sterilization process takes advantage of high-pressure steam at high temperatures which is maintained for a set time period. Correct operation of autoclaves is essential since improper use may result in incomplete sterilization which poses risks of contamination and hospital-acquired infections (HAIs). Medical equipment suppliers who master these operational steps help clients use devices properly while meeting health regulations and establishing trust in equipment reliability.
Medical environments prioritize infection control because reusing instruments without adequate sterilization creates major health hazards. Autoclaves deliver a reliable sterilization approach that safeguards patients and staff from infectious pathogens. Dealers and distributors should focus on educating clients about autoclave operation because this knowledge helps clients understand its significance in achieving regulatory compliance and maintaining healthcare safety.
A comprehensive step-by-step guide explains the process of using an autoclave properly.
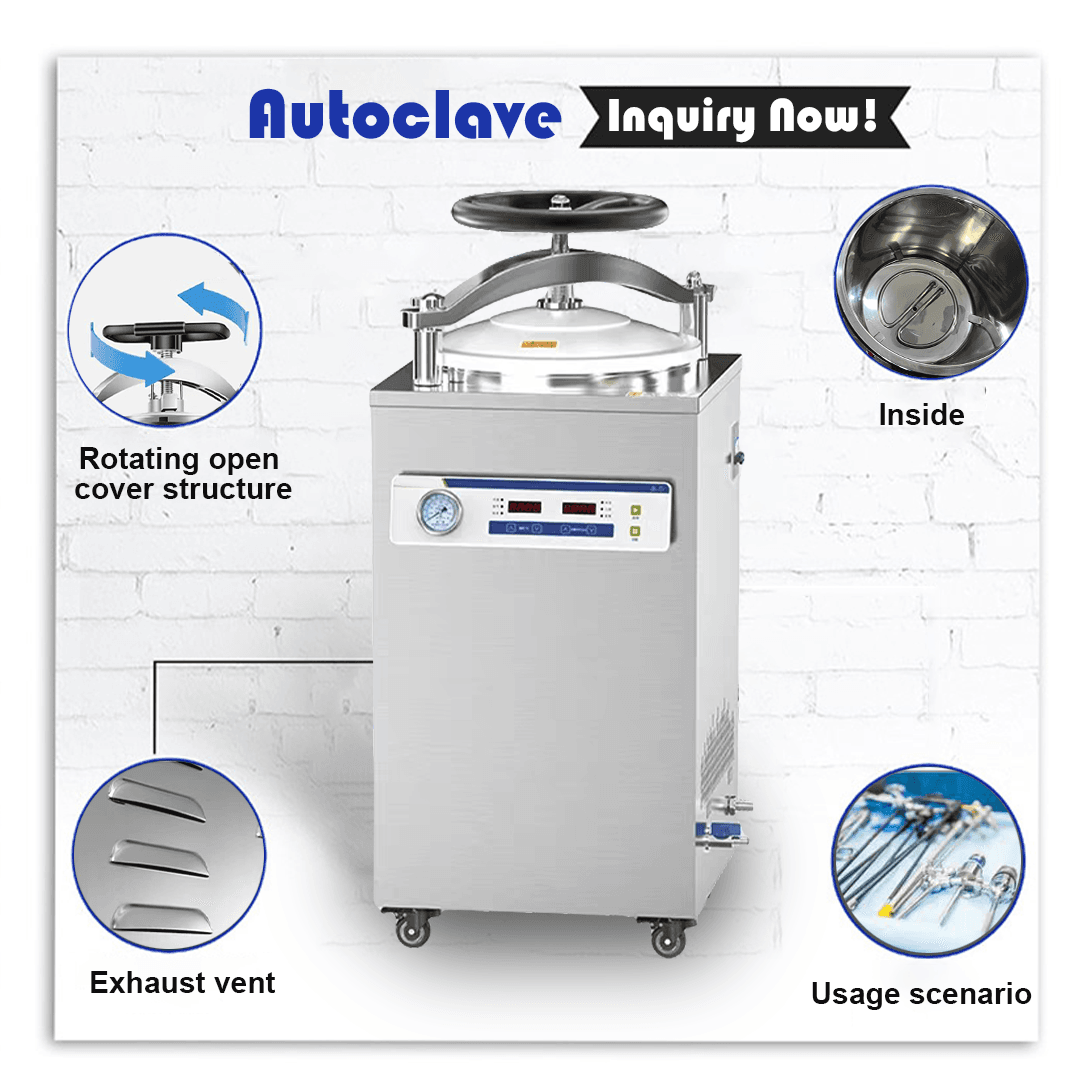
Safe and effective autoclave operation requires users to study its components and control interface before usage. The majority of autoclave units feature a sealed chamber for item containment, steam generation heating systems, pressure control mechanisms and a control panel for selecting operational parameters such as temperature settings and cycle duration. Read the user manual and operational guidelines for your model to recognize essential functions such as start/stop buttons, cycle selection options, and safety indicators. Autoclave suppliers who deliver explicit operational instructions or training sessions enable clients to effectively use control systems which prevents misuse and boosts user confidence for proper sterilization performance.
The correct preparation of items represents the essential initial stage when operating an autoclave. The first step of sterilization requires meticulous cleaning of instruments because any residue of debris or organic material acts as a protective barrier for pathogens against steam heat reducing the effectiveness of sterilization. Disassemble all multi-part tools to fully expose surfaces when possible and make sure every item can withstand high temperatures and moisture ranging from 121°C to 134°C. When items require sterility post-cycle choose proper packaging options like sterilization pouches or wraps. Teaching clients proper autoclave usage through correct item preparation helps dealers prevent operational mistakes and achieve reliable sterilization outcomes while enhancing their support services.
Proper loading of the autoclave chamber ensures all items receive consistent steam and heat during the sterilization process. Keep the chamber from becoming too full because overcrowding can block steam access and reduce sterilization effectiveness. Stack items in the autoclave with proper spacing between them and use trays or racks if available to enable steam circulation around every object. Store weighty objects on the bottom shelves while positioning light and heat-sensitive materials above them to prevent damage. Position wrapped or packaged items in a way that prevents obstruction of vents or drainage systems. Distributors should train clients in autoclave loading techniques to achieve optimal performance while avoiding incomplete sterilization which builds trust in equipment reliability.
The proper water level is vital when operating an autoclave because most devices use water to produce steam for sterilization. Make sure to examine the reservoir or chamber and fill it with distilled or deionized water according to recommendations because tap water contains minerals that can lead to buildup and impact performance. Avoid overfilling because excess water can cause both operational problems and safety risks. Modern autoclaves often include automatic water filling systems which make this task easier. Autoclave suppliers provide clients with guidance on selecting proper water quality during training sessions which extends equipment life and maintains sterilization performance.
Understanding the appropriate sterilization cycle selection is essential for effective autoclave operation because specific material types and load conditions require precise temperature, time, and pressure settings. General instruments require standard sterilization at 121°C for 15–30 minutes under 15 psi whereas unwrapped tools can be processed more quickly at 134°C for 3–10 minutes with 30 psi pressure. To select the appropriate sterilization cycle for your load type—unwrapped, wrapped, or liquid—you should consult operational guidelines or facility protocols. Medical equipment professionals who deliver precise instructions on cycle selection to their clients can prevent autoclave operation mistakes while ensuring effective sterilization for all types of materials.
After loading the chamber and adding water seal the autoclave door tightly to ensure an airtight space required for pressure build-up and high temperature generation. Follow the locking mechanism specific to your autoclave model because some require manual latches while others operate with automatic locking systems. Make sure no items or packaging block the seal because leaks will hinder the establishment of proper sterilization conditions. Dealers who focus on this step when training autoclave users will help their clients prevent safety hazards and operational problems while guaranteeing effective sterilization results.
Begin the sterilization cycle by pressing the control panel buttons after verifying that the door is securely shut in the autoclave operation procedure. Activate the sterilization cycle by pressing the start button or by confirming the selected settings based on your specific model. Real-time data displays for temperature, pressure and remaining time enable operators to track the sterilization process. Only interrupt the cycle when absolutely necessary because doing so may compromise sterility and force you to restart the entire process. Through display monitoring of autoclave cycles distributors can train clients to confidently operate the equipment and handle any issues during use.
Throughout the autoclave cycle maintain active supervision to ensure that all operating parameters stay within the defined limits which include temperature between 121°C and 134°C and pressure from 15 to 30 psi according to the programmed time. Modern autoclave units come with integrated safety mechanisms including alarms and automatic shutoff systems which activate during pressure drops or overheating incidents. Avoid opening the door while the autoclave functions because hot steam release could lead to serious burns. Suppliers must educate clients about autoclave operation with an emphasis on safety protocols to avoid accidents and comply with safety regulations while enhancing equipment reliability.
Do not open the autoclave door immediately after sterilization completes because opening it too soon will release hazardous steam that could cause burns. During the depressurization and cooling phase many units undergo pressure and temperature reduction until they reach safe levels. Only proceed when the indicator or display shows it’s safe which happens when internal pressure reaches zero and temperature declines substantially. Dealers who teach clients about the cooling phase of autoclave usage help prevent injuries and maintain sterilized items’ quality which leads to improved satisfaction for users.
Ensure the autoclave has cooled before opening the door to remove sterilized items with heat-resistant gloves or tools that protect against burns caused by remaining heat. Check items for moisture and damage because wet packs suggest incorrect loading or cycle settings which require reprocessing. Transfer unwrapped items directly to a sterile setting or keep wrapped items closed until they need to be opened to preserve sterility. Distributors who teach clients proper autoclave unloading techniques enable them to keep their instruments sterile and satisfy infection control regulations.
Effective autoclave operation requires post-cycle cleaning and maintenance to maintain its long-term performance. To prevent water accumulation inside the autoclave chamber or reservoir, empty all remaining water and use a non-abrasive cloth to cleanse the interior surfaces. Perform regular checks of gaskets, seals, and vents for signs of wear and damage since these elements influence both sealing capabilities and pressure retention. Perform regular maintenance checks to calibrate the temperature and pressure sensors to maintain their accuracy. Maintenance support and spare parts provision by suppliers during autoclave training enables clients to maintain optimal equipment conditions while establishing strong long-term trust.
Effective autoclave operation confirmation requires using chemical or biological indicators during the autoclave usage process. Chemical indicators show color shifts under precise temperature and time conditions while biological indicators check for viable spores following the cycle. Quality assurance protocols require documentation of results to maintain health regulation compliance. Medical equipment professionals must teach clients autoclave validation methods to emphasize verification’s importance which results in consistent sterilization outcomes and meeting audit standards.
Operating an autoclave demands utmost safety awareness due to the extreme temperatures and pressures it produces. Protect yourself from burns and steam exposure by wearing suitable personal protective equipment including heat-resistant gloves, safety goggles, and lab coats. Operators must receive proper training to safely handle both hot materials and pressurized conditions. By advising clients on safety equipment for autoclave operations dealers show client care which strengthens the appeal of their products.
Operating an autoclave exposes workers to the frequent risk of burns from hot steam and surfaces. Opening the autoclave door during a cycle or immediately after completion should be avoided until the machine has sufficiently cooled down and the pressure has been released. Take necessary precautions during unloading because remaining heat may result in injuries. The device should be situated in an area with good airflow to help it release heat effectively. By teaching clients the essential precautions for autoclave use distributors enable them to reduce risks while keeping their facilities safe.
Even when proper care is taken, autoclaves may experience malfunctions that include pressure leaks and temperature failures. Learn emergency shutdown procedures thoroughly to prepare for incidents and maintain access to troubleshooting guides at all times. Users should halt the operating cycle when a malfunction occurs but only if it remains safe to stop and then reach out to technical support for help. Clients gain preparedness for autoclave emergencies through supplier-provided emergency protocols which maintain both safety standards and sterilization effectiveness.
When operating an autoclave avoid common mistakes that can lead to operational failures.
Autoclave users frequently overfill the chamber which blocks steam circulation and results in insufficient sterilization. Respect the recommended load capacity guidelines and maintain proper item spacing during use. Equipment reliability is reinforced for dealers by teaching clients how to avoid operational failures and achieve consistent results through proper autoclave usage training.
People frequently make operational errors with autoclaves when they choose an incorrect sterilization cycle for the items being processed. Heat-sensitive materials will be damaged by a short cycle with high temperature while resistant pathogens may not be sterilized because of inadequate time or temperature settings. Always follow the provided guidelines to choose correct settings for the materials processed. Through reference charts and cycle selection training distributors assist clients with autoclave operations to prevent mistakes and ensure effective results.
Performance issues like mineral buildup and seal degradation occur when autoclaves are not maintained regularly which affects sterilization effectiveness. Maintain consistent autoclave operation by following a regular schedule to drain water and clean the chamber while inspecting each component. Equipment vendors deliver maintenance programs and service options for autoclave operation which enable clients to maintain peak performance and maximize equipment longevity.
Performing sterilization without using chemical or biological indicators may lead to unnoticed sterilization failures which present contamination risks. Through proper testing methods verify sterilization processes and keep records to meet compliance standards. Medical equipment professionals who emphasize proper validation procedures for autoclave operation support their clients in maintaining quality standards and preventing health risks within their facilities.
Mastering how to work an autoclave is a vital skill for medical equipment dealers, distributors, and procurement specialists who support healthcare providers in achieving effective sterilization. By following the detailed steps—from preparation and loading to cycle selection, monitoring, and maintenance—you can ensure that autoclaves deliver reliable results in eliminating pathogens and safeguarding patient safety. Adhering to safety precautions and avoiding common mistakes further enhances operational success, while validation confirms the efficacy of each cycle. As a trusted provider, staying informed about best practices in working an autoclave positions you to offer invaluable guidance to clients, helping them meet infection control standards with confidence. If you’re ready to explore high-quality autoclave solutions or have questions about their operation, we’re here to assist. Contact us via email, WhatsApp, or visit our website at https://autoclaveequipment.com/ for expert advice and tailored solutions to meet your clients’ sterilization needs.
Basic steps include preparing items by cleaning, loading the chamber correctly, adding water, selecting the appropriate cycle, sealing the door, starting the process, monitoring safety, cooling down, unloading safely, and maintaining the device.
Proper operation ensures complete sterilization of medical instruments, preventing infections and meeting health regulations critical for patient and staff safety in healthcare settings.
Wear protective gear like heat-resistant gloves and goggles, avoid opening the door during operation, allow cooling before unloading, and follow emergency protocols for malfunctions to prevent injuries.
Avoid overloading the chamber, using incorrect cycle settings, neglecting maintenance, and skipping validation of sterilization results, as these can compromise efficacy and safety.
Ensure proper loading, select the right cycle for the load type, monitor parameters like temperature and pressure, validate results with indicators, and maintain the device regularly for consistent performance.
Validation using chemical or biological indicators confirms that sterilization was successful, ensuring no pathogens remain and maintaining compliance with quality and safety standards in medical environments.
Contact Us for Expert Advice and Solutions Looking to source reliable autoclaves for your clients? Reach out to us today for personalized support!
Email: inquiry@shkeling.com
WhatsApp: +8618221822482
Website: https://autoclaveequipment.com/
We’re excited to assist you with all your sterilization equipment needs!

Healthcare facilities must adhere to rigorous hygiene and sterilization standards without exception. Medical equipment distributors and procurement professionals must understand the tools that maintain standards to deliver value to healthcare
Maintaining sterile medical tools and equipment stands as the most important practice for preventing infections and ensuring patient safety in healthcare settings. Medical equipment distributors along with dealers and procurement

The fast-paced healthcare sector operates under strict regulations which demand that sterility maintenance stands as a primary concern to protect patient safety and ensure compliance with operational standards. Medical equipment
Sterilization equipment serves as an essential tool in healthcare settings to maintain cleanliness standards and protect patients. Medical equipment distributors together with dealers and procurement specialists need to know the
Autoclaves serve as essential components of sterilization processes in healthcare facilities through high-pressure steam to destroy pathogens on medical instruments and other materials. Medical equipment distributors and procurement specialists must

Healthcare environments must prioritize sterilization because it protects patients and staff by removing infectious pathogens from medical devices and materials. The autoclave stands out as one of the best tools