
This article provides an in-depth exploration of autoclaving sterilization, including its definition, process steps, effectiveness, and essential safety considerations. Designed for medical device distributors, dealers, and procurement professionals, this guide will empower you to make informed decisions and ensure the highest standards of safety and compliance for your clients.
The method of Autoclaving sterilization requires high-pressure saturated steam at high temperatures to eliminate all living microorganisms such as bacteria, viruses, fungi, and spores. The autoclave device generates a controlled pressurized environment necessary for comprehensive sterilization during the process.
Both “autoclaving sterilization” and “autoclave sterilization” are terms referring to an identical fundamental sterilization process. Various professional and regulatory standards identify autoclaving sterilization as the best practice for decontaminating reusable medical devices and laboratory equipment alongside other materials.
Autoclaving sterilization is critical for maintaining infection control standards and meeting regulatory requirements while ensuring patient safety. Hospitals, clinics, laboratories, and manufacturing settings depend on this process to maintain essential sterility standards. The process meets international standards and stands as a fundamental element of present-day healthcare and life sciences research.
Do autoclaving sterilization and autoclave sterilization define the same procedure?
Autoclaving sterilization and autoclave sterilization represent identical sterilization procedures. The terms describe the sterilization process achieved by using an autoclave which applies moist heat under pressure. The terminology difference between the two terms exists only semantically since scientific and regulatory literature accept both terms.
Autoclaving sterilization emphasizes the action or process.
Autoclave sterilization highlights the equipment used.
Proficient communication with regulatory bodies and healthcare professionals requires familiarity with both terms across global client bases. Technical documentation along with procurement specifications and compliance guidelines both frequently include these terms.
For further reading, see:
All items require complete cleaning to eliminate organic matter and debris before undergoing sterilization.
All instruments and materials enter autoclaves through sterilization wraps or pouches that preserve their sterile condition post-processing.
The autoclave chamber must contain items arranged to allow enough room for steam to flow freely.
Overloading is avoided to prevent incomplete sterilization.
Sterilization cycle parameters including temperature, pressure, and duration depend on both the type and number of items being processed.
Standard sterilization cycles function at a temperature of 121°C (250°F) and a pressure of 15 psi over a duration of 15 to 30 minutes.
The sterilization process uses elevated temperature cycles such as 134°C/273°F for specific applications.
The autoclave first removes air from the chamber and then fills it with saturated steam.
Steam reaches every surface to provide even heat distribution.
The sterilization process uses heat and pressure to denature proteins and break down cell membranes which results in the destruction of all microorganisms.
The cycle time is carefully managed to achieve total sterilization.
The sterilization cycle finishes when it vents steam from the chamber while resetting pressure to atmospheric levels.
Autoclaves with drying phases help prevent moisture retention.
Sterilized items undergo removal with sterile technique and proper storage to preserve their sterile condition until usage time.
Autoclaving sterilization has been scientifically established to eradicate every category of microbial life including highly resilient bacterial spores.
Biological indicators like spore strips together with chemical indicators such as autoclave tape validate the effectiveness of the sterilization process.
Autoclaving sterilization provides consistent results every time and complies with healthcare and laboratory international standards.
Only trained personnel should operate autoclaves.
Wear personal protective equipment including heat-resistant gloves, goggles, and lab coats.
Users must exercise caution when opening the autoclave door after a cycle because residual steam and heat might cause burns.
Ensure the chamber is not overloaded to maintain proper steam flow.
Wait for items to cool down before touching them to prevent burn injuries.
Autoclave operation depends on consistent maintenance routines that involve inspecting gaskets and calibrating systems while keeping the chamber clean.
Malfunctioning autoclaves should be serviced immediately.
Not all materials are suitable for autoclaving. Heat-sensitive plastics along with volatile chemicals and electronic devices should never go through the autoclaving process.
Always check manufacturer guidelines for compatibility.
Keep comprehensive records for all sterilization cycles which document both parameters and the results from biological/chemical indicators.
Organizations need complete documentation to meet regulatory standards and ensure quality control.
The sterilization method of autoclaving stands as the foundation for preventing infection and maintaining quality standards across medical, laboratory, and industrial fields. The method stands as the top choice for sterilizing critical instruments and materials because of its exceptional effectiveness and reliability while adhering to global standards. Medical device distributors along with dealers and procurement professionals who understand autoclaving sterilization and its safe usage can achieve maximum safety levels with complete client satisfaction and full regulatory compliance.
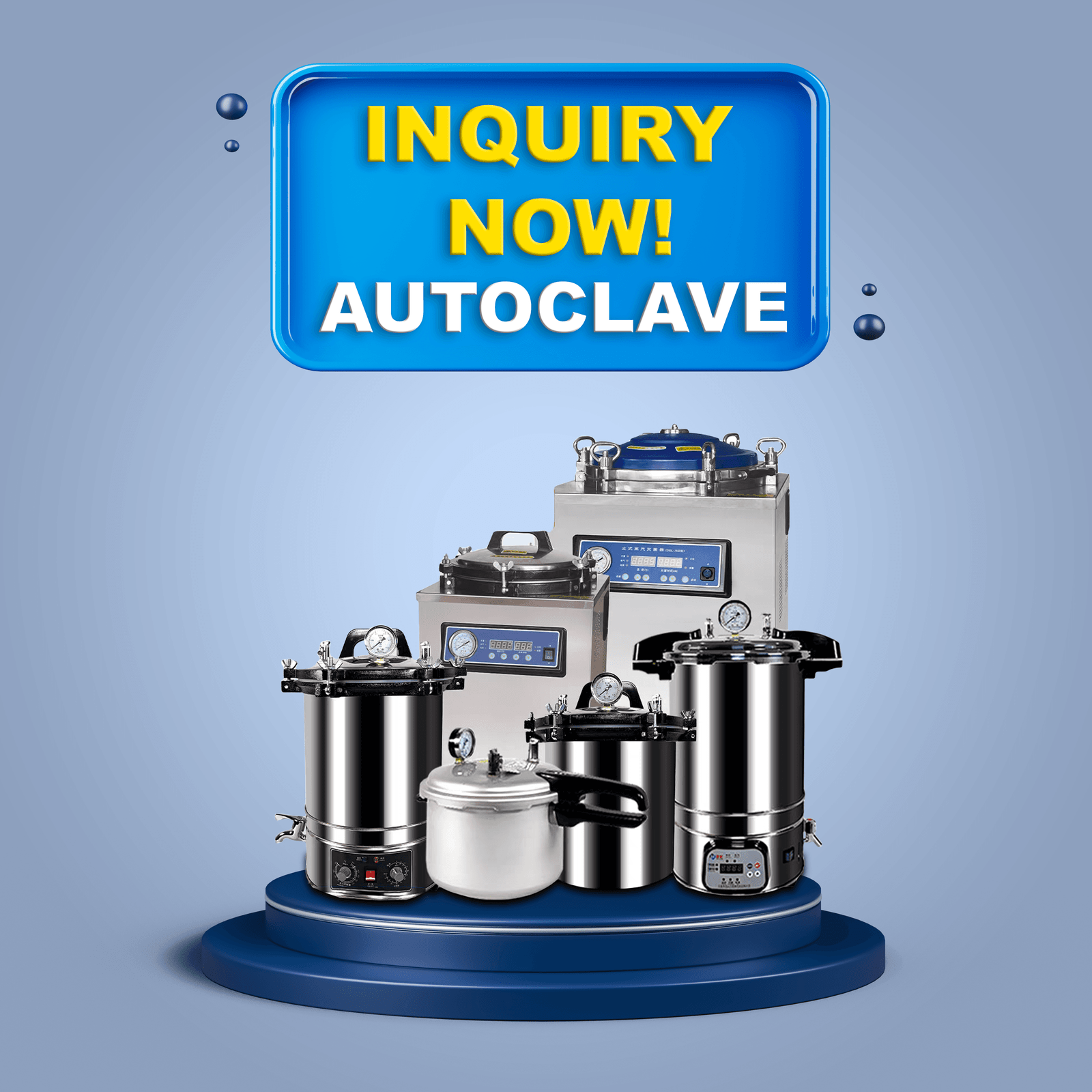
Our experienced team stands ready to provide you with expert guidance and advanced autoclave solutions specifically designed for your business needs.
Autoclaving sterilization is the process of using high-pressure steam in a sealed chamber to kill all microorganisms on instruments and materials, making them completely sterile.
Autoclaving sterilization uses moist heat under pressure, making it faster and more effective than dry heat or chemical methods for most reusable medical and laboratory items.
Commonly autoclaved items include surgical tools, laboratory glassware, media, textiles, certain plastics, and biohazardous waste.
Yes, items sensitive to heat or moisture, certain plastics, volatile chemicals, and electronic devices should not be autoclaved.
You can find more information at ما هو التعقيم بالأوتوكلاف؟ و What is Autoclaving?.
Are you searching for reliable autoclave solutions or professional advice on sterilization for your business? Our expert team is here to help with tailored recommendations and support.
البريد الإلكتروني: inquiry@shkeling.com
واتساب: +8618221822482
الموقع الإلكتروني: https://autoclaveequipment.com/
Contact us today for a consultation or quote, and let us help you achieve the highest standards of sterilization and safety!
يجب أن تعطي بيئات الرعاية الصحية والمختبرات الأولوية للإزالة الكاملة للكائنات الدقيقة الخطرة من جميع المعدات والمواد كخطوة حاسمة في حماية سلامة المرضى والسيطرة على العدوى. التعقيم بالتعقيم الأوتوماتيكي

تعمل صناعة الرعاية الصحية بموجب لوائح صارمة وتتطلب تعقيم الأدوات الطبية لحماية المرضى من العدوى والحفاظ على معايير السلامة. يشكل جهاز التعقيم بالأوتوكلاف القوي المكون الأساسي لـ
تعتبر أجهزة الأوتوكلاف ضرورية في مجال الرعاية الصحية لأنها تعمل على تعقيم الأدوات والمواد الطبية مما يساعد في السيطرة على العدوى. تحدد الصيانة الدورية إلى جانب التنظيف المناسب ما إذا كانت هذه الأجهزة ستعمل بفعالية. الأجهزة الطبية

تعد أجهزة التعقيم من المعدات الأساسية في مجال الرعاية الصحية ومكافحة العدوى للحفاظ على تعقيم الأدوات الطبية ومعدات المختبرات إلى جانب المواد الحيوية الأخرى. موردو المعدات الطبية وخبراء المشتريات

يجب على مقدمي الرعاية الصحية إعطاء الأولوية لتعقيم الأدوات والمواد للوقاية من العدوى وحماية صحة المرضى بشكل فعال. وقد أثبت التعقيم بالأوتوكلاف أنه طريقة يمكن الاعتماد عليها بشكل استثنائي وتستخدم على نطاق واسع في جميع أنحاء

تتطلب صناعة الرعاية الصحية تدابير صارمة لمكافحة العدوى، وبالتالي فإن بعض الشروط والأدوات ضرورية لضمان السلامة والنظافة. في البيئات الطبية والمعملية التي تتطلب ظروفًا معقمة