
This FAQ article covers all essential questions regarding autoclave operation as well as safety protocols and troubleshooting methods. If you are beginning to learn about autoclaves or you want to advance your knowledge base this resource will offer essential insights to benefit your business operations and customer support.
Medical, laboratory and industrial settings use autoclaves for sterilizing multiple types of equipment. These include:
The autoclave sterilizes medical tools like scalpels, forceps, scissors, retractors and other reusable metal instruments.
Beakers, flasks, pipettes, and test tubes represent essential laboratory glassware.
Autoclaves can sterilize surgical textiles including drapes and gowns but only if they are marked as autoclave-safe.
Autoclavable labels indicate specific types of tubing, syringes, and containers made from rubber and plastic materials.
Laboratory media like agar plates and broth solutions fall under Culture Media and Solutions.
Biohazardous waste includes contaminated dressings along with laboratory disposables.
Nota: Not all materials are suitable for autoclaving. Heat-sensitive materials like certain plastics as well as electronics and delicate instruments risk damage when exposed to autoclaving processes. Check manufacturer instructions for every item before using the autoclave.
The duration of an autoclave cycle varies based on item type and quantity alongside the chosen cycle and specific autoclave model. Typical cycle durations include:
Standard Gravity Cycle (121°C): 30–40 minutes
Pre-Vacuum Cycle (134°C): 15–20 minutes
The Liquid Cycle duration ranges from 30 to 60 minutes based on both the volume of material and the type of container used.
Wrapped or porous loads require 10–30 minutes drying time which is essential for their proper sterilization.
Additional Factors:
The chamber requires additional time to reach safe handling temperatures during the warm-up and cool-down phases.
Heavier or denser loads need extended cycle durations to achieve thorough steam distribution.
Due to their operation at elevated pressures and temperatures autoclaves demand strict safety measures. Essential safety precautions include:
Training: Only trained personnel should operate autoclaves.
Use heat-resistant gloves together with lab coats and eye protection during autoclave loading and unloading operations.
Place items in a way that promotes steam flow while preventing excessive loading.
Make sure the door shuts completely and locks before activating the autoclave cycle.
Select the program that matches the type of load you are sterilizing.
The door should remain closed until the pressure gauge displays zero and the chamber reaches a safe temperature.
Maintain the autoclave through scheduled inspections and servicing to keep all safety mechanisms operational.
A combination of high-pressure steam with controlled elevated temperature exposure time allows autoclaves to destroy all microbial life forms including bacteria, viruses, fungi, and spores. The process involves:
The air removal process involves evacuating all air from the chamber to enable steam to reach every surface.
The sterilization process requires steam to access every section of the load for complete sterilization.
The exposure phase requires maintaining validated temperature and pressure levels for a specific period.
Monitoring Methods:
The physical monitoring approach includes digital displays and printed cycle parameters.
Chemical indicators utilize color-changing tapes and strips to verify exposure to steam.
Spore tests offer the most reliable confirmation of sterilization effectiveness.
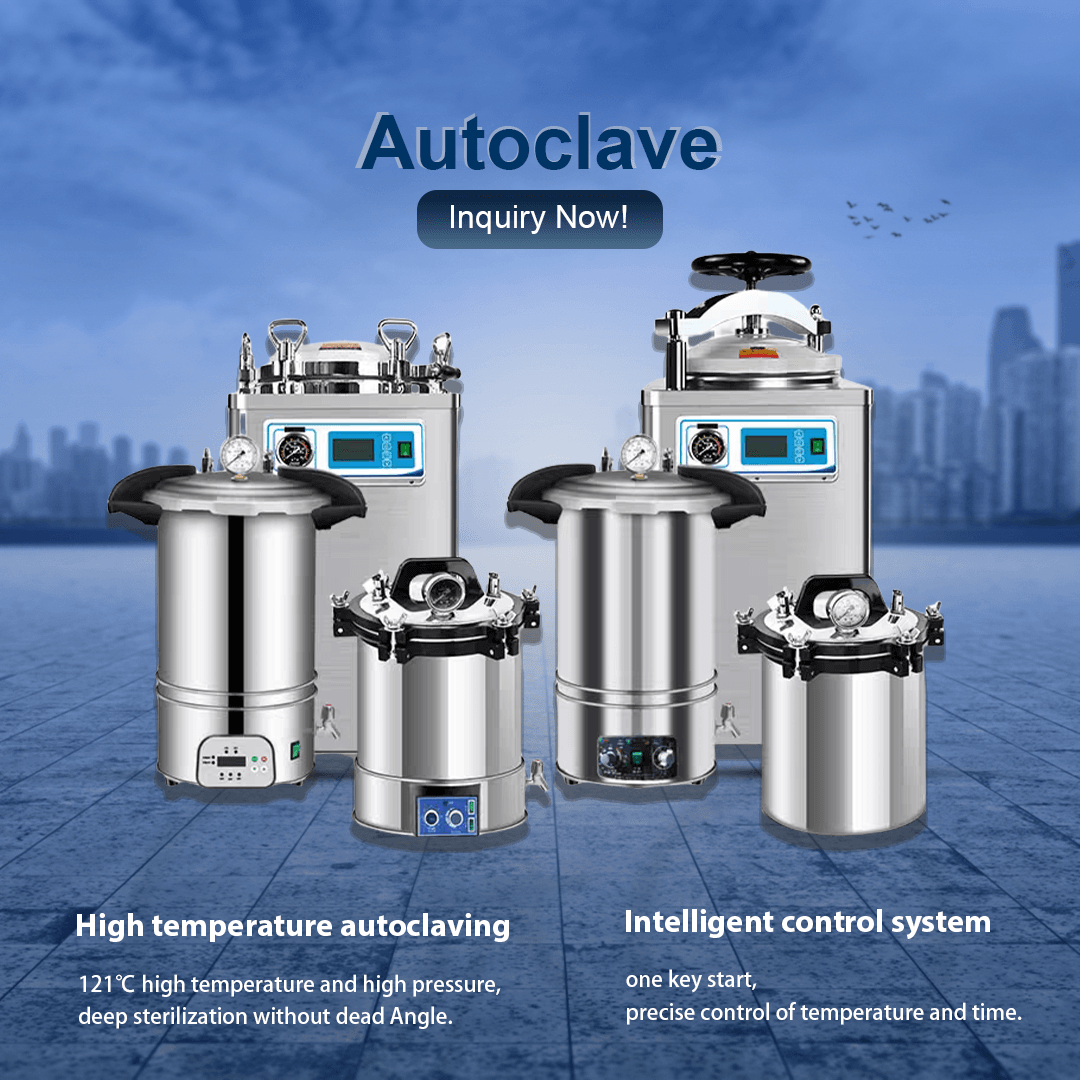
Multiple autoclave models exist which match various specific applications.
Gravity Displacement Autoclaves utilize steam to push out air with gravity’s help and are best suited for uncomplicated sterilization tasks.
Pre-Vacuum (High-Vacuum) Autoclaves utilize a vacuum pump to remove air from the chamber before introducing steam to achieve deeper penetration in porous or wrapped materials.
Tabletop Autoclaves are small sterilization devices meant for medical clinics and laboratory settings.
Large capacity autoclaves serve hospitals and central sterilization departments as well as industrial applications.
Autoclaves have the capability to sterilize various types of liquids including culture media as well as saline solutions and laboratory chemicals. Autoclaves utilize special liquid cycles with reduced heating and cooling rates to avoid boiling over and achieve uniform sterilization.
For safety during autoclaving procedures use vented caps on containers and avoid overfilling them while allowing extra cooling time before removing them.
In case the autoclave cycle does not complete correctly because of power outages or temperature/pressure problems or incomplete sterilization then perform these actions:
All items that were processed during a failed cycle should be considered non-sterile.
To find the problem you need to examine error messages, analyze logs and search for machine defects.
Once you’ve fixed the problems, reload the autoclave and execute a fully validated cycle.
Keep records of the incident to fulfill quality assurance requirements and regulatory compliance obligations.
Autoclaves may still experience problems despite operating according to guidelines. Here are some common problems and solutions:
Sterilization failures can occur due to overloading the autoclave or using improper packaging methods along with insufficient air evacuation or not running the exposure cycle long enough.
To resolve issues reduce load size then repack items next check blocked vents and finally verify cycle parameters.
The sterilization cycle failed to properly dry the items because of an insufficient drying phase length or too much moisture from the load or premature chamber door opening.
Ensure full drying cycle completion by extending drying time and reducing load moisture before opening.
The chamber retaining pressure combined with a malfunctioning door lock mechanism can cause this issue.
Allow pressure to drop to zero before checking the gauges and using the user manual for troubleshooting guidance.
The autoclave might present issues due to sensor errors or power problems along with maintenance requirements.
Use the autoclave manual for guidance, perform regular maintenance checks and get technical support when needed.
The cause of chamber odors or residue can be traced back to organic material build-up or improper cleaning procedures.
Approved solutions should be used to clean the chamber consistently and items must be pre-cleaned before undergoing sterilization.
For foundational knowledge and step-by-step process details, refer to:
Autoclaves are indispensable tools for ensuring the sterility of medical and laboratory equipment. By understanding how autoclaves work, what can be sterilized, process durations, safety precautions, and troubleshooting methods, distributors, dealers, and procurement professionals can make well-informed decisions and provide valuable support to their clients.
Regular training, strict adherence to validated protocols, and routine maintenance are essential for maximizing the effectiveness and safety of autoclave operations. Staying informed about best practices will help you uphold the highest standards of infection control and regulatory compliance in your field.
If you have further questions or need expert guidance on selecting or maintaining autoclaves, our team is ready to assist you.
For expert advice, custom solutions, or to discuss your autoclave requirements, contact us today: Correio eletrónico: inquiry@shkeling.com WhatsApp: +8618221822482 Sítio Web: https://autoclaveequipment.com/
Our specialists are dedicated to supporting medical device distributors, dealers, and procurement professionals with advanced autoclave technology and personalized service. Reach out now for a consultation or quote!

Sterilization standards in veterinary healthcare must remain flawless to protect both animals and veterinary professionals. The specialized vet autoclaves designed to sterilize instruments and equipment used in animal care fulfill

Autoclaves are recognized as the top choice for sterilization practices which protect healthcare settings while keeping medical instruments free from pathogens. Autoclave temperature functions as a key determinant in sterilization

The healthcare and veterinary sectors depend on sterilization as an essential safety procedure with autoclaves serving as the fundamental equipment for this critical operation. The autoclave temperature serves as the

Autoclaves serve as the primary method for sterilization in healthcare and veterinary environments to ensure safety and hygiene. Medical professionals frequently ask about the appropriate sterilization duration for unwrapped items

As instalações de cuidados de saúde têm de aderir a normas rigorosas de higiene e esterilização, sem exceção. Os distribuidores de equipamento médico e os profissionais de aprovisionamento têm de compreender as ferramentas que mantêm as normas para fornecer valor aos cuidados de saúde
A manutenção de ferramentas e equipamentos médicos esterilizados é a prática mais importante para prevenir infecções e garantir a segurança dos doentes em ambientes de cuidados de saúde. Os distribuidores de equipamento médico, bem como os comerciantes e os compradores